SIBO 101: Signs & Associated Conditions
- Dr. Nazanin Safaei, ND, MS

- Jun 27, 2025
- 6 min read
Updated: Jul 10, 2025

Small Intestinal Bacterial Overgrowth (SIBO) is a gastrointestinal condition that has gained increasing attention due to its connection with a variety of chronic symptoms and diseases. SIBO occurs when bacteria more commonly found in the colon abnormally increase in the small intestine. This microbial imbalance can significantly affect digestion, nutrient absorption, and overall health.
What Is SIBO?
Under normal conditions, the small intestine contains relatively low levels of bacteria compared to the large intestine. In SIBO, this balance is disrupted, and excessive bacteria—often types that are native to the colon—colonize the small intestine. These bacteria ferment carbohydrates prematurely, leading to gas production and gastrointestinal symptoms [1]. The overgrown bacteria in the small intestine also competes with the host for nutrients, and some more invasive types can cause inflammation and damage to the bowels lining.
Signs and Symptoms of SIBO
SIBO can manifest in a wide array of symptoms, many of which overlap with other digestive and non-digestive disorders [2]:
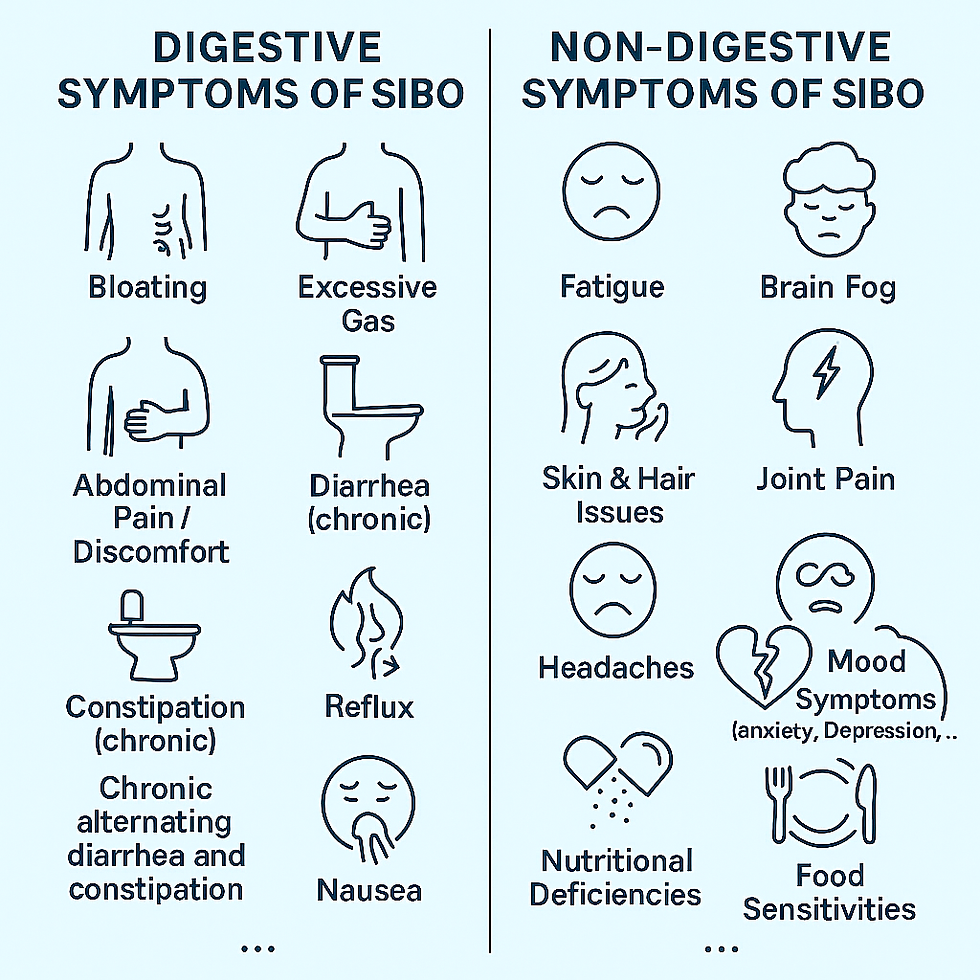
Because these symptoms are non-specific, SIBO is often misdiagnosed or overlooked.
Conditions That Can Open the Door to SIBO
SIBO may occur as a secondary complication of other medical conditions that affect gut motility or the structure of the gastrointestinal tract. These include:
Irritable Bowel Syndrome (IBS): A significant number of IBS patients test positive for SIBO, especially those with diarrhea-predominant IBS [3]. On the other hand, SIBO may also lead to symptoms of IBS.
Celiac Disease: Even with a gluten-free diet, some individuals continue to have gastrointestinal symptoms due to SIBO [4].
Hypothyroidism: Decreased gut motility can contribute to bacterial overgrowth [5].
Diabetes Mellitus: Particularly type 1 and long-standing type 2 diabetes, due to their adverse effect on the nervous system affecting motility [6].
Crohn’s disease and other structural abnormalities, including adhesions and diverticula [7].
Chronic use of proton pump inhibitors (PPIs) and opioids, which can alter gut pH or motility [8]. PPIs are medications that reduce stomach acid production.
Gastroparesis or Motility Disorders: Impaired gut transit increases SIBO risk due to bacterial stasis [13]
Common Co-Existing Conditions
Untreated SIBO may play a role in the development or exacerbation of the following conditions:

Irritable Bowel Syndrome (IBS): Up to 78% of IBS patients test positive for SIBO using breath tests [14]. It is debated that IBS can both lead to or be caused by SIBO.
Rosacea: SIBO has been associated with higher prevalence in patients with rosacea, and treatment may improve symptoms [18].
Chronic Fatigue Syndrome (CFS): Overlap may be due to mitochondrial dysfunction, inflammation, and gut dysbiosis [16].
Fibromyalgia: Many fibromyalgia patients have positive SIBO breath tests; treating SIBO may reduce symptoms [15].
Irritable Bowel disease (Crohn’s, Ulcerative Colitis): SIBO is more prevalent in patients with IBD, especially those with strictures or surgery [17].
Non-Alcoholic Fatty Liver Disease (NAFLD): Increased endotoxin load from SIBO can impair liver metabolism and contribute to fat deposition [19].
Rheumatoid Arthritis (RA): SIBO may play a role in the development or exacerbation of RA through mechanisms involving gut dysbiosis, systemic inflammation, and immune dysregulation. SIBO can promote intestinal permeability ("leaky gut") and systemic endotoxemia, which are believed to contribute to autoimmune activation in genetically predisposed individuals [20,21,22,23].
Interstitial cystitis/bladder pain syndrome (IC/BPS): The gut-bladder axis suggests that SIBO-induced dysbiosis and increased intestinal permeability may promote systemic inflammation and contribute to bladder hypersensitivity. Studies show a higher prevalence of SIBO and IBS among patients with interstitial cystitis, pointing toward a shared pathophysiology and the potential benefits of addressing SIBO in IC management [24,25,26,27].
Restless Leg Syndrome: cause may be related to systemic effects of SIBO, including nutrient deficiencies and inflammation [28].
Systemic Inflammation: caused by transfer of bacterial toxins, also called LPS, into circulation promoting chronic inflammation [29].
Conclusion
SIBO is a complex and often underdiagnosed condition that can severely affect a person's quality of life. Recognizing the signs and conditions associated with it is a crucial first step toward getting the right diagnosis and support. If the symptoms sound familiar, it may be time to dig deeper into what’s really going on in your gut. In our next post, SIBO 102: Diagnosis and Treatments, we’ll explore how SIBO is diagnosed and the most effective ways to treat it—so stay tuned as we continue the path to better digestive health.
Disclaimer: The information provided in this article is for informational and educational purposes only and is not intended as medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider before making changes to your diet, lifestyle, or health care regimen.
References
Grace E, Shaw C, Whelan K, Andreyev HJN. Small intestinal bacterial overgrowth (SIBO): A systematic review of diagnostic methods. Gut. 2013;62(5):741-752. doi:10.1136/gutjnl-2011-302190
Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial overgrowth: A comprehensive review. Gastroenterol Hepatol (N Y). 2007;3(2):112-122.
Pimentel M, Lembo A, Chey WD, et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364(1):22-32. doi:10.1056/NEJMoa1004409
Tursi A, Brandimarte G, Giorgetti GM. High prevalence of small intestinal bacterial overgrowth in celiac patients with persistence of gastrointestinal symptoms after gluten withdrawal. Am J Gastroenterol. 2003;98(4):839-843. doi:10.1111/j.1572-0241.2003.07390.x
Lauritano EC, Gabrielli M, Lupascu A, et al. Small intestinal bacterial overgrowth and irritable bowel syndrome-related symptoms in hypothyroidism. Am J Gastroenterol. 2007;102(4): 828-832. doi:10.1111/j.1572-0241.2007.01113.x
Gabrielli M, D’Angelo G, Di Rienzo T, et al. Prevalence of small intestinal bacterial overgrowth in type 2 diabetes: Correlation with metabolic control and intestinal motility. J Clin Endocrinol Metab. 2013;98(2):E379-E383. doi:10.1210/jc.2012-3164
Rana SV, Bhardwaj SB. Small intestinal bacterial overgrowth. Scand J Gastroenterol. 2008;43(9):1030-1037. doi:10.1080/00365520801947852
Lombardo L, Foti M, Ruggia O, Chiecchio A. Increased incidence of small intestinal bacterial overgrowth during proton pump inhibitor therapy. Clin Gastroenterol Hepatol. 2010;8(6):504-508. doi:10.1016/j.cgh.2009.12.022
Rezaie A, Buresi M, Lembo A, et al. Hydrogen and methane-based breath testing in gastrointestinal disorders: The North American Consensus. Am J Gastroenterol. 2017;112(5):775-784. doi:10.1038/ajg.2017.46
Khoshini R, Dai SC, Lezcano S, Pimentel M. A systematic review of diagnostic tests for small intestinal bacterial overgrowth. Dig Dis Sci. 2008;53(6):1443-1454. doi:10.1007/s10620-007-0055-2
Pimentel M, Fadul R, Lembo A. Rifaximin therapy for IBS: A review of clinical efficacy and safety in the target population. Ther Adv Gastroenterol. 2020;13:1756284820912976. doi:10.1177/1756284820912976
Staudacher HM, Irving PM, Lomer MCE, Whelan K. Mechanisms and efficacy of dietary FODMAP restriction in IBS. Nat Rev Gastroenterol Hepatol. 2014;11(4):256-266. doi:10.1038/nrgastro.2013.259
Quigley EMM. Small intestinal bacterial overgrowth: Roles of antibiotics, prebiotics, and probiotics. Gastroenterology. 2019;156(6):1515-1519. doi:10.1053/j.gastro.2018.12.019
Pimentel M, Chow EJ, Lin HC. Eradication of small intestinal bacterial overgrowth reduces symptoms of irritable bowel syndrome. Am J Gastroenterol. 2000;95(12):3503-3506. doi:10.1111/j.1572-0241.2000.03356.x
Pimentel M, Wallace D, Hallegua D, et al. A link between irritable bowel syndrome and fibromyalgia may be related to small intestinal bacterial overgrowth. Ann Rheum Dis. 2004;63(4):450-452. doi:10.1136/ard.2003.013813
Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018;9(6):162. doi:10.1038/s41424-018-0030-7
Shah SC, Day LW, Somsouk M, Sewell JL. Meta-analysis: the association between small intestinal bacterial overgrowth and inflammatory bowel disease. Aliment Pharmacol Ther. 2019;49(6):634-643. doi:10.1111/apt.15163
Parodi A, Paolino S, Greco A, et al. Small intestinal bacterial overgrowth in rosacea: clinical effectiveness of its eradication. Clin Gastroenterol Hepatol. 2008;6(7):759-764. doi:10.1016/j.cgh.2008.02.054
Boursier J, Mueller O, Barret M, et al. The severity of NAFLD is associated with gut dysbiosis and shift in the metabolic function of the gut microbiota. Hepatology. 2016;63(3):764-775. doi:10.1002/hep.28356
Bjarnason I, Helgason KO. Gastrointestinal permeability and bacterial translocation in rheumatoid arthritis. Gut. 2000;46(4):498-500. doi:10.1136/gut.46.4.498
Fasano A. Leaky gut and autoimmune diseases. Clin Rev Allergy Immunol. 2012;42(1):71-78. doi:10.1007/s12016-011-8291-x
Zhang X, Zhang D, Jia H, et al. The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med. 2015;21(8):895-905. doi:10.1038/nm.3914
Mönkemüller K, Fry LC, Rickes S. NSAID-induced enteropathy. Curr Treat Options Gastroenterol. 2006;9(5):386-396. doi:10.1007/s11938-006-0024-5
Rosen JM, Klumpp DJ. Mechanisms of pain from urinary tract infection. Int J Urol. 2014;21 Suppl 1:26-32. doi:10.1111/iju.12335
Cozean CD, Cozean LA. Treating interstitial cystitis with an anti-inflammatory diet. Urol Nurs. 2007;27(6):531-537.
Chiu B, Tai T, Chung S. Gastrointestinal disorders in patients with interstitial cystitis/bladder pain syndrome. Tzu Chi Med J. 2018;30(4):222-225. doi:10.4103/tcmj.tcmj_1_18
Ueda T, Hanno P, Saito R, et al. Clinical phenotyping of interstitial cystitis/bladder pain syndrome: a review of current evidence and future perspectives. Int J Urol. 2021;28(1):12-26. doi:10.1111/iju.14362
Weinstock LB, Walters AS. Restless legs syndrome is associated with irritable bowel syndrome and small intestinal bacterial overgrowth. Sleep Med. 2011;12(6):610-613. doi:10.1016/j.sleep.2010.10.002
Miele L, Valenza V, La Torre G, et al. Increased intestinal permeability and tight junction alterations in nonalcoholic fatty liver disease. Hepatology. 2009;49(6):1877-1887. doi:10.1002/hep.22848
©2025 by Nazanin Safaei, ND, MS